“I really want a hamburger!”
by Brian Wright
 [Previous: Omamacare V]
[Previous: Omamacare V]
On Wednesday early a.m., 1/23/13, Mom was short of breath and her pulse was racing by my feel. She eventually insisted on going to ER (I had actually become inured to her seeming out of breath and was balking at taking her in!!). We arrived at emergency about 9:00 or 10:00 a.m.
The ER physician saw her fairly quickly and because pulse was remaining high w/nitro and other meds, he suggested entubation to enable breathing with ventilator assist; I agreed (not fully realizing the ramifications). At ~1300 she was moved—unconscious, because sedative is used for inserting the tube—to ICU. This is where Omamacare VI starts. Mother, unconscious, is basically breathing with ventilator assistance in ICU, while ICU diagnoses the root problem. I’m a bit foggy on events and personnel in this early hospitalization timeframe.
I’m going in every morning trying to catch the rounds and get a series of ICU doctors and PAs who seem quite knowledgeable and communicative. Nursing staff seems generally ‘OK’ except for a young lady who does a ‘Me Jane You Nobody’ imitation. Initially over the telephone, I had to brush her back to let her know who the customer is in this situation and that she would be better off listening more and barking orders less. Fortunately, I don’t have to deal with her subsequently; whenever I visit and she’s present around the nurses’ bullpen, she frantically avoids eye contact.
But for three-five days we are waiting for test results and for her to reach a state where they can remove the vent tube. [For the longest time I was concerned that Mom was not going to come back to consciousness and I forget what it was that we needed to do or she needed to be before they would pull the vent tube. Eventually, we saw some response and her numbers (pulse, oxygen, BP) were good enough that they extubated.] I want to say it isn’t until 1/30 for the extube. She moves to general hospital quarters I think ~1/28, or maybe it’s the same day as extube.
Anyway by Friday 1/25 they know Mom has no infection and no blood clot in the lungs. Also, originally I had thought maybe all she needed was dialysis, but the XRays taken back in ER on the 23d showed no fluid in the lungs. IOW her respiratory failure this time is because of a heart failure, heart racing, paroxysmal afib, not able to get oxygen to cells to lungs, etc. Her heart ‘Ejection Fraction’—a measure of the efficiency of the heart pump—from the echocardiogram taken in the ER was a mere 12-15%!
Same day as ER entube, in ICU, Mom’s pulse was lowered and stabilized using Cardizem, a calcium channel blocker, with the Coreg maxed out. [Later changed to Amiodarone before discharge.]
They extubated, she’s in general, they insert the NG tube for feeding via nose into the stomach and for meds. I remember again being concerned that she would not regain awareness. But finally her eyes started to open I want to say in ~2/1/13, Friday. And there was increasing response. [Nurse Ted in ICU told me that coming out sometimes takes a long time. His father, a state senator—after winning or losing an election, I forget which—was unconscious for weeks.] Then on 2/4 they removed the NG tube (annoying temporary feed tube via the nose) and inserted the PEG tube (permanent feeding tube into the stomach), using a procedure requiring anesthetic. [She’s being dialyzed regularly, I would say an average of four per week.]
Assessment
My evaluation of the care process is from the perspective of two qualities I regard as key to any health care ‘system:’ continuity and connection. Now isn’t the time for a detailed paper, but consider the graphic below:
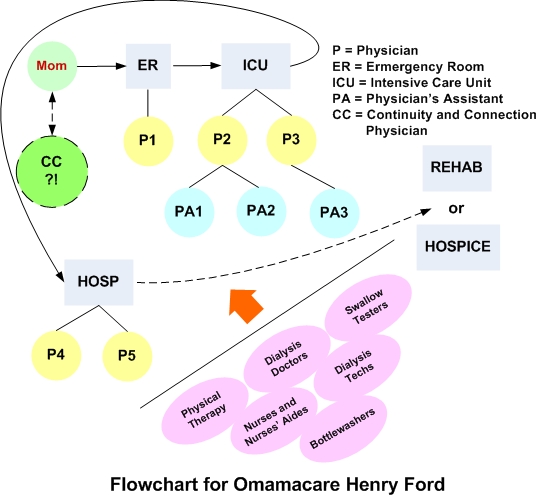
The question of the hour is a) how does the system work now, and b) how to make it better. You can see for now, there exist far too many cooks and bottlewashers, an assembly-line approach where the individual (Mom in this case) is passed from one station to the next. Then at the end of the line the final physician gathers all his or her notes recorded by the whole team to make the diagnosis and treatment—not to mention physicians’ assistants, nurses, nurses aides, auxiliary physicians (e.g. dialysis or nephrology specialists), and so on, who have had a hand.
Not to put too fine a point on it, but Henry, as topnotch as he is relative to the competition, is still piece o’ meat, bloodletting, true-care-free medicine: Nobody has fundamental responsibility or sayso for the well being of the patient-customer. I include a Continuity and Connection Physician (CC) button in my graphic with a big question mark. Something to think about. Who has fundamental responsibility?! A big reason for any superior care for a particular individual is whether he or she has an advocate like me; but the current system makes even the advocate job trying by having so many fluctuating points of contact vs. one.
As it stands now, too many people exist up and down the line who have little incentive to put their skin in the game. How do you cure that? My experience is the doctors are most dedicated and focused, but they are hampered by the pass-the-baloney, hot-potato approach to medicine. It’s too easy for the nursing and other staff to simply go through the motions, show up and do their time. Still I note several instances of individual excellence breaking out from exceptional people in all the disciplines… which is the one virtue of the current corporate system (despite itself) that a complete government system (Obamacare) will totally cast aside.
What’s Next?
Rose is over to visit on 2/3, Sunday, and brings the Teddy Bear. Mom still subdued and only voicing a little. (Reason for PEG tube is that swallow test negative. Takes a while for valve to recover and reseat, even for youth.) Finally on Friday 2/8 afternoon she’s discharged to the Manor o’ Love. [This is actually the Manor of Novi where Mom rehabbed following her minor stroke in August of 2012. I call it the Manor o’ Love because you can actually feel the special care of the people there for everyone.] She really hasn’t recovered any strength, been lying in a hospital bed for 15 days, still spacey from residual drugs of the anesthetic on 2/4. IOW, Mom has spent the great majority of two weeks recovering from insertion of the vent tube!!
She’s dialyzed on 2/9 Saturday, very weak coming in, perking up leaving. Sunday and Monday not much change. PT and OT at Manor, can only do so much. Plus it’s the weekend. Tuesday 2/12 dialysis is a repeat of Saturday. Wednesday 2/13 the Manor pushes the panic button based on 82% oxygen and sends Mom back to ER. Rehab does not do acute care. It was almost going to be Providence Hospital, a tad closer, which would have been a disaster. Just lucky Sade called me and I insisted Mom be transported to Henry Ford West Bloomfield.
 So where am I, where am we? Mom and me. I have power of attorney for her and am the executor of her estate, meager as it is; I also have healthcare power of attorney, which while a person is alive and under care of a medical establishment is the gold standard of consideration. Basically, this means I decide whether to continue medical intervention into my mother’s dimming light. And it’s a hard call. The Do Not Resuscitate (DNR) decision—is easy enough, because it basically tells the interventionists not to insert a breathing tube or attempt to do CPR (which at my mom’s age of 86 would likely entail death anyway by breaking bones of the rib cage).
So where am I, where am we? Mom and me. I have power of attorney for her and am the executor of her estate, meager as it is; I also have healthcare power of attorney, which while a person is alive and under care of a medical establishment is the gold standard of consideration. Basically, this means I decide whether to continue medical intervention into my mother’s dimming light. And it’s a hard call. The Do Not Resuscitate (DNR) decision—is easy enough, because it basically tells the interventionists not to insert a breathing tube or attempt to do CPR (which at my mom’s age of 86 would likely entail death anyway by breaking bones of the rib cage).
 But what’s difficult is you don’t want to let go. I want her health back, I want her back. Since she’s come back from the hospital, and gone to dialysis and back from the rehab nursing home, she’s not recovered anything like the energy level she had previous to the respiratory attack. The photo on the right shows her lethargy on the Monday after coming back from the hospital, the day before dialysis, when I had hoped the Manor could get started with her physical and occupational therapy… you know get her on to the first rung of the recovery ladder so she can get back to where she was. I’m sure these feelings are normal.
But what’s difficult is you don’t want to let go. I want her health back, I want her back. Since she’s come back from the hospital, and gone to dialysis and back from the rehab nursing home, she’s not recovered anything like the energy level she had previous to the respiratory attack. The photo on the right shows her lethargy on the Monday after coming back from the hospital, the day before dialysis, when I had hoped the Manor could get started with her physical and occupational therapy… you know get her on to the first rung of the recovery ladder so she can get back to where she was. I’m sure these feelings are normal.
It’s difficult to let go of the vision of health, or even relative health, where one has a walking, talking, thinking, lovely creature who, though declined and no longer able to care for herself or himself, is ‘there’ and there for you. I am so not prepared to let that vision go, not without a fight. I grasp at straws: for the previous week I come to ascribe Mom’s down-and-out manner as a consequence of the anesthetic used in the insertion procedure for the PEG tube. As one without appreciable kidney function, she would not be able to remove drug toxins without dialysis. And she’s been in bed for 15 days, too! SO DIALYSIS AND EXERCISE WILL BRING MY MOM BACK FOR SURE… only it isn’t happening.
The nephrologist finally shows up around 1830 in the ER, where Mom has been scheduled for general admittance. Mohindras is the ideal physician. She asks a few questions, comes up with what seems yet another obvious conclusion to hang on to, that Mom is not getting the nourishment she needs. Dr. Nephro is going to see to it some supplements are added to Mom’s PEG tube tonight, and dialyze tomorrow. So HOPE! Once again. This has to be the answer, Mom’s not getting enough food energy to reach the first rung on the recovery ladder. We’ll get her well and back to rehab, then in no time she’ll be coming home, making salads, and feeding the cat.
Then, icing on the cake. As if to confirm my newfound hope, Mom, who’s only spoken a handful of complete sentences during the past three weeks, lights it up with an aside to  me right there in emergency: “I really want a hamburger!” Then off she goes, admitted to to general quarters, around 21:00.
me right there in emergency: “I really want a hamburger!” Then off she goes, admitted to to general quarters, around 21:00.
… and that night getting to my car in the parking lot is a lot quicker by air!
[Omamacare VII: Rehab or Hospice (to be continued)]
This post has been read 1749 times!