Rites of final passage
by Brian Wright
 We left it in the previous incarnation of Omamacare (VI) that I was walking on air, with a view to having found that magic bullet—it was to be nutrition that would bring Mom back to full function, symbolically in her stated desire for a simple hamburger—to keep her going. Sadly, no sooner had I taken sleep and nourishment back at home then returned to the hospital next day (Valentine’s Day of all days), that my hopes were dashed. Lying in the bed there in luxo-suite C341, she’s being dialyzed and showing no real signs of thriving. Still, I hope to see improvement after dialysis and rest, with another hit of the enhanced nutrients, later in the day.
We left it in the previous incarnation of Omamacare (VI) that I was walking on air, with a view to having found that magic bullet—it was to be nutrition that would bring Mom back to full function, symbolically in her stated desire for a simple hamburger—to keep her going. Sadly, no sooner had I taken sleep and nourishment back at home then returned to the hospital next day (Valentine’s Day of all days), that my hopes were dashed. Lying in the bed there in luxo-suite C341, she’s being dialyzed and showing no real signs of thriving. Still, I hope to see improvement after dialysis and rest, with another hit of the enhanced nutrients, later in the day.
Backing up a few days, on Monday 2/11, while I’m signing the admission papers for Mom at the Manor of Novi, the admissions officer notifies me that their default funeral home for transport of the body in case of death is so and so down the street. I had checked them out in early February to find out their cremation costs (~$2000 seems to be the standard funeral home price). I did some preliminary search for alternatives in early Feb, not improving much on the price—The American Way of Death is definitely a state-controlled, i.e. privileged, industry.
It’s occurring to me on 2/11 that Mom may actually be closer to the end than I had been assuming. Thus, I resume my search that very day for reasonably priced cremation—Mom has already designated that she will be cremated and has a plot in the Oakwood Cemetery in Allegan, Michigan, alongside her mother, father, and, soon, one of her sisters. Fortunately, I locate a full-service home, Generations of Farmington Hills, which keeps its costs and prices low by concentrating 95% of its business on cremation. It will be roughly $700, including copies of the death certificate.[1] I’m glad to finally discharge this concern from my mind so I can focus on the present.
The next day, Wednesday 2/13, her respiration percentage declines to less than 90% at the Manor and we have to take Mom to ER—which I already have written up in Omamacare VI. So fast forward now again to the morning of Valentines Day 2/14/13. This is the morning I confer with the latest staff physician from the hospital ward and read thru Mom’s rap sheet:
Acute hypoxemic respiratory failure due to acute pulmonary edema due to paroxysmal atrial fibrillation (afib) w/rapid ventricular rate (RVR) in setting of congestive heart failure (CHF), severe mitral-valve regurgitation (MR), severe tricuspid-valve regurgitation (TR)—ejection fraction (EF): 12%—and end-state renal disease (ESRD); severe oropharyngeal dysphagia, aphonia, and hoarseness following extubation; presbycusis with wide bowing of bilateral vocal folds and very large posterior glottic gap upon attempted phonation; Deconditioning; clostridium difficile (C-Diff.) diarrhea.
Reminds me of the old joke: there’s a handbill circulated for someone’s lost dog: “blind in one eye, has three legs, is missing his right ear, had his tail run over, was accidentally neutered. Answers to the name ‘Lucky.'”
From my perspective, Mom is still on the cusp of possible recovery. She’s alert, though doesn’t talk much, except when she first sees me come in the room. She’ll say something like, “Good morning, I’m feeling okay.” But the remainder of the time, it will be nods and shakes of the head; it probably causes her discomfort to talk, and it’s easier not to.
After conferring with the staff physician, I chat with Henry Ford Hospice Nurse Chuck and agree to set up an appointment for Friday to have a final discussion of hospice and sign the papers for Mom to be admitted ‘there’… as opposed to any further attempts to pursue rehab. We talk enough that I’m pretty sure they’re right—the doctors and Chuck—that Mom is not responding to enhanced nutrition, that there are simply too many ‘morbidities’ to ignore. Mom has what they call multiorgan dysfunction syndrome (MODS). Plus her albumin level is 2.4, beneath the threshold of 2.5, which suggests a possible terminal condition of no longer being able to gain nourishment from food.
I arrive back at the hospital that night around 6:00 or 7:00, after Mom has rested from dialysis, and we have the discussion about hospice vs. rehab. I put it on the line as gently as I can, basically telling her with some background that I’ve been gathering that if she gets discharged from the hospital back to rehab, the chances are close to 100% that she’ll fail to meet the oxygenation threshold for acute care (90%) and rehab will slap her back on a gurney, destination ER… for as many cycles as the heart can tolerate, which probably won’t be many. Plus they’ll continue to dialyze, poke and prod, etc.
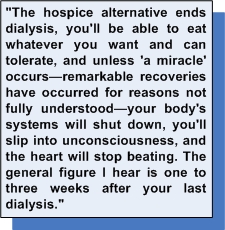
I say, “The hospice alternative ends dialysis, you’ll be able to eat whatever you want and can tolerate, and unless ‘a miracle’ occurs—remarkable recoveries have occurred for reasons not fully understood—your body’s systems will shut down, you’ll slip into unconsciousness, and the heart will stop beating. The general figure I hear is one to three weeks after your last dialysis.” Then I ask what she wants.
She tells me clearly with a full voice, “I choose hospice.”
I brought a DVD and a laptop computer to play it on. It’s the perfect Netflix choice: The Waltons. Season 1, Disc 1. Mom is relatively lively and attentive for the whole first episode. It fits: The Waltons starts out on a farm in 1930s Virginia; Mom grew up in the 1930s on a farm in the Danish community of Greenville, Michigan. [When you stop and think for a spell about the problems of the world, application of the moral code of Waltons’ Mountain would solve nearly 90% of them, in a New York Minute.]
 On Friday morning, 2/15, I sit down with Hospice Nurse Chuck again and sign the papers. Mom is designated into a temporary internal hospital care situation called ‘respite,’ which according to Medicare, as I understand it, is limited to five days. Chuck assures me that the effective day for start of respite will be Sunday, meaning that Mom can remain in the hospital until Friday, 2/22. As of Saturday 2/16, the Henry Ford internal hospice physicians and nursing staff will be the ones monitoring Mom’s condition.
On Friday morning, 2/15, I sit down with Hospice Nurse Chuck again and sign the papers. Mom is designated into a temporary internal hospital care situation called ‘respite,’ which according to Medicare, as I understand it, is limited to five days. Chuck assures me that the effective day for start of respite will be Sunday, meaning that Mom can remain in the hospital until Friday, 2/22. As of Saturday 2/16, the Henry Ford internal hospice physicians and nursing staff will be the ones monitoring Mom’s condition.
Right out of the gate that weekend I get good feedback from the attending hospice physician that Mom is doing great, has an appetite, no excessive fluid buildup, blood pressure fine, oxygenation 95%+, seems aware and content, even more conversational. Hosannah Danna Danna! Maybe a miracle will occur. After so many years of invasive or interventionist medicine—dialysis, fistula surgeries, hospitalizations and ERs, medications, dealing with other organ declines, whatever is causing persistent lethargy and faintheadedness, etc.—I hold out renewed hope that a liberation from pokes and prods will cause her system to spontaneously right itself. The photo above, with Mom holding the Teddy Bear Rose brought for her, gives you an idea of why hopes are high.
Hospice, Hospice
On Monday the 18th I begin meeting with the Henry Ford Hospice (HFH) social workers and performing other tasks to make sure all the bases are covered in the event of Mom’s passing. After all, the idea of hospice is care and comfort during a person’s period of passage into the Great Beyond. This is the week for two things: a) wrangling out the details of hospice care, and b) spending as much quality time as I can in the hospital with my one and only Mama Bear—basically each day could be her last.
Those final few nights in the hospital—where I show up, chat with her, and and put on a Waltons episode—I try to touch all the bases for her connections to her ‘warm center of life’ that I can… family, friends, her cat, Tabby, nature, fond shared memories, etc.
Family. Yes, I do need to discuss this briefly. Where are they? Mom had three children: myself and another son and a daughter. We all live in Michigan. My brother, who died in 2007, fathered three children and my sister bore four children. I don’t have any children… yet. So besides me, familywise, Mom has a daughter and seven grandchildren, now in their 20s and early 30s—four great-grandchildren, too. You would think Mom’s direct descendants, most living inside a radius of 60 miles, would have taken the effort—from the start of her dialysis in 2009 and through her three previous hospitalizations (heart attack 10/6/11, heart attack 10/31/11, and stroke 8/1/12)—to at least occasionally contact her and send her well wishes. They know her email address, phone number, where she dwells… also my contact information.
On those previous occasions I made a point of updating the grandchildren on her condition, soliciting supportive calls, visits, email, etc. on Mom’s behalf. [I did not contact my sister or my brother’s widow because they had strongly and explicitly excommunicated me, and Mom collaterally, in that period.][2] Not a peep. Zero, zilch, nada. Whatsa matta wit kids today, huh? Understand that Mom has been the exemplary loving-not-meddling grandmother to these young ‘uns as they were growing up: babysitting, gifting, writing letters, providing airfare and accommodations in a couple of cases of extended visits, and all the quality time that entails.
This time around, in consultation with Mom, I decide not to inform her daughter or any of the direct descendants of Mom’s situation. At this 11th hour, we can’t afford any wild cards. The inevitability of an ‘unfinished business’ scene at mom’s expense is too great a risk in her condition. I would never forgive myself for allowing the possibility of emotional toxins into the caring, loving surroundings I’ve tried to cultivate for my weakened mother’s final passage. No one has to tell me how metaphysically sad it is that such a wonderful woman as Phyllis Joy Wright will likely end her days with 1/8th the descendent family she deserves at her bedside.[3]
As for the wrangling with hospice, I’m becoming increasingly unhappy with them. For one thing, Mom has to be out of hospital respite by Thursday, not Friday as I was assured by Nurse Chuck. I have to make the decision on a facility sooner than I expected. I had talked with one social worker on Friday; this week it’s a different social worker , and she’s not particularly accommodating. More like a drill sergeant telling me “how it’s gonna be, pretty boy;” won’t listen to protestations. I’m don’t have enough energy to raise the issue to the next level of decision making, so I just let it go and go through the list of facilities that Mom’s plan covers.
It’s at this time—roughly Tuesday February 19—that it dawns on me that home hospice is probably the best deal. It’s covered by insurance, they install the equipment in your home, and supposedly the hospice care nurses and aides come out at regular intervals. [Important note: for most Medicare-supplemental plans, hospice care is covered but ROOM AND BOARD IS NOT. So somehow I would have to figure out where to come up with the several thousand dollars for placing her in a facility. (Most hospice residences want a month’s room and board up front.)] Duh, why did I even think of not bringing her home with me: familiar surroundings, her cat, TV, I’ll be there 24/7, etc.?! I can’t believe my denseness; also, I have to wonder why Social Workers don’t suggest home hospice from the gitgo.
That’s it, then. Problem solved. Next. Well, not quite, as it turns out. I have expectations that whatever I need to know will be conveyed by the hospice staff at handoff. Shouldn’t I be receiving some training? On Wednesday I clean up my condo, clearing out a spot on the bottom floor; that night I spend maybe an hour at the hospital with Mom in her room. She’s not improving, in fact, each night she seems to be less fully conscious and communicative. But she still smiles when she sees me and as I kiss her on the forehead to say goodbye. I so hate to leave her there with strangers. She’s going to be coming home. Yes!
Thursday afternoon, February 21, 2013, is one of the major discouraging events in my life. The ambulance has brought her home from the hospital, and instead of looking better, she looks, well, like death warmed over. She’s pale as the sheets on the gurney. [There was some later discussion with people in hospice that in her condition it was a mistake to move her out of the hospital; hospice nurses talk of time remaining in 1) weeks to months, 2) days to weeks, and 3) hours to days. She’s a ‘3’ but no one tells me that. I’m still of the mindset she’s a ‘2’ or even a ‘1.’] What of my expectations that she’ll get better, start talking, be with me for a few weeks?
Also, where is my hospice handoff nurse? What am I supposed to do here? I get on the phone. An hour or two later the hospice nurse arrives. Quite a bit of equipment has preceded Mom’s arrival: a bed, oxygen machinery, commode, medical supplies like diapers, sheets, eating tray, etc. I get some training from Delivery Guy on the bed and the oxygen. Handoff Nurse brings some other supplies, but medications are her priority. She walks me through the meds; points me to the diapers, sheets, and gloves; and talks in general terms about giving Mom nourishment and cleaning her up. No hands on training for the latter.
 Mom is vaguely aware of her surroundings, but is not recovering much color. She can nod and shake her head, but mainly she sleeps. Our cat, Tabby, occasionally lands on Mom’s new bed, but generally is anxious about the goings-on and stays upstairs; Tabby shows no signs of knowing this is the woman on whose bed Tabby still sleeps after a month of the Mama Bear’s absence. I’m concerned that I don’t know enough to take care of the situation, and say so to Handoff. My understanding is that a hospice nurse will be coming out tomorrow, Friday, but Handoff says no. Also, nurses only come once a week. Mine isn’t scheduled until Monday! Aides may come as many as five times a week, but generally only twice a week. Hey, this can’t be right!
Mom is vaguely aware of her surroundings, but is not recovering much color. She can nod and shake her head, but mainly she sleeps. Our cat, Tabby, occasionally lands on Mom’s new bed, but generally is anxious about the goings-on and stays upstairs; Tabby shows no signs of knowing this is the woman on whose bed Tabby still sleeps after a month of the Mama Bear’s absence. I’m concerned that I don’t know enough to take care of the situation, and say so to Handoff. My understanding is that a hospice nurse will be coming out tomorrow, Friday, but Handoff says no. Also, nurses only come once a week. Mine isn’t scheduled until Monday! Aides may come as many as five times a week, but generally only twice a week. Hey, this can’t be right!
Handoff takes some time to look Mom over, says things don’t look great, and I forget why I didn’t raise a flag on that or call the hospice emergency number. Handoff is really a sweet and caring person. I’m such a sap! Over the few hours Mom has been home and in the bed, she has seemed to get better, her color improving, the skin warming. Also she’s eating small amounts. Handoff leaves. I put on a Waltons‘ episode; Mom sleeps through most of it. I set up the hideabed to be able to sleep downstairs for the night. Mom seems to forcefully clear her throat a lot, until she’s fully asleep; I keep her head and upper body slightly elevated per (someone’s) instructions to help against the congestion.
Friday is just a waiting and attending operation. Rose comes over later in the day. When Mom is awake I give her her meds on the schedule and try to feed her, but she’s constantly sleeping and has little appetite. She has been off dialysis for a full week now. The day passes uneventfully. I’ve made arrangements with a private home health aide named Irene to come out Saturday to clean Mom up. Irene was referred by Sally, a sympathetic soul at HF Hospital WB who runs a tea kiosk in the atrium with her husband.
Saturday. Irene is a sturdy older woman, old school, compassionate and hardworking. She tells me that many times she’s left a hospital because the staff there just went through the motions and didn’t give the care or attention people deserved. My kinda woman. And she shows me how to clean and take care of Mom in the bed, which Mom needs at this time. Okay, that’s how that’s done. I’m beginning to get more and more pissed that nobody from HFH saw fit to bring me up to speed on the basics. Having someone as competently caring as Irene has renewed my spirit if not my hopes.
Sunday, February 24, is a watershed day. Mom opens her eyes in the a.m. She’s chewing and swallowing, I think. According to “Signs of Approaching Death” that HFH gives me, she’s moved from the ‘Up to 72 Hours Remaining’ to perhaps the ‘Preactive Phase: About 2 Weeks Remaining’ condition. Mostly Mom sleeps and tries to clear her throat. Thankfully, Rose has come over in the early afternoon and stays ’til 8:00. At roughly 3:00 p.m. I feel Mom has had enough of the congestion coughing up and gurgling. I call the on-call HFH nurse. This turns out to be the right thing to do. I should have done it two days earlier.
On-Call first orders us a suction device to take care of that coughing. [The same guy who brought the bed brings the suction system, shows me how to use it, and it’s a big winner. A couple of applications and Mom is no more laboring trying to clear her throat.] On-Call also realizes how incapable I am of dealing with Mom’s needs, especially in the delivery of meds. She decides to pay a personal visit: I learn how to crush pills between two spoons instead of using a hammerhead on the counter, she shows me how to use the big syringe to deliver the meds thru Mom’s PEG tube (tube that goes directly into her stomach), and, most important, to get Mom on the right meds.
OC, a straight shooter, tells me Mom is in the ‘hours to days remaining’ timeframe. We need to go to pain and comfort meds, now. Particularly the morphine derivative, but also a drug that prevents the congestion. I get the impression that the mission has become—and perhaps should have become a few days ago (OC is the one who suggests that if it were her decision, she would never have discharged Mom from the hospital)—to let Mama drift off into LaLa Land. My job is simply to keep the happy-lever primed and apply water-moistened swabs to Mom’s mouth, which dries out because of the congestion med and because it’s been staying open for breathing.
Since Mom has been home, I’ve had the sense she really doesn’t want to wake up and assume the full routine of consciousness. The new regime of medications basically grants her wish. She isn’t smiling exactly, but compared to her sleep of the previous days and nights, her look is contented and pain free. Believe it or not, I still feel that she can buck the odds and in her pain-free state spontaneously spring back to life. The dim prospect keeps me from appreciating the sad fact that her awareness is probably forever gone from my world. February 24th is Academy Award Night. I watch, resigned, with Mom ‘somewhere else’ in the other bed.
Monday, a truly fine HFH nurse’s aide shows up, having the same name as the on-call nurse. From her I learn additional information about how to move about people in bed, change them, clean them; there’s a lot of applied engineering involved. I learn she has a son in the Detroit school system, and mention Marva Collins, the free-lance educator who founded a street academy in Chicago and taught inner-city kids reading, writing, and arithmetic at college levels. I was really glad to know her; she brightened my day. Only meds for Mom now, no food. A different HFH nurse arrives this afternoon, whom I recognize from the hospital. She is Mom’s case nurse.
Tuesday, February 26. Nurses Aide comes back, does her Mom maintenance work in the morning, then leaves. Mom continues in a steady-state condition. Approximately 1:30 I go upstairs to do some paperwork, an editing job, or an article. After 2:00 I come downstairs again, then notice Mom’s loss of color, thinking, “Well, dammit, this looks bad,” and come closer listening for breathing. I check for pulse, the skin is cool. I make the call to Case Nurse. She comes out and confirms. Mom is gone.
Modest Exit
Several steps have to take place now, some of which I need to be part of. So the grieving and tears take turns with waiting for the police to show up, answering some questions, then waiting for the funeral people to come and retrieve the body. It’s just beginning to snow and sleet vigorously. Case Nurse is a gem, young and attractive, a real plus for me now as I want desperately to feel the promise and hopes of human life, not its aging and loss. What’s more, she’s the perfect sympathetic ear, fully professional and engaging while letting me babble on about this and that, in between the frequent intervals of serious ‘moist-eye syndrome.’
[On the several occasions I’ve cried since my mom entered the hospital a month ago, I’ve tried to be aware of what causes it. Something wells up from the inside; there’s no thought behind it. And then it goes away as quickly as it comes and you can actually form intelligible sentences, come back into rational control. You realize something about crying is quite good, probably because it is so honest and biological; it makes you know you’re alive. Of course, the sadness means failure of a kind. Who wants that? The trick is to learn from the deep emotion, come into a correspondingly profound sense of connection to Being, to existence, to your true soul, and to the person you have lost. Indeed, that is my experience with Mom.]
And now, as Paul Harvey says, The Rest of the Story:
I’ll spare the reader recounting my emotional turmoil the next several days and the sadness of so many others she knew and loved upon hearing of her death. Universally, they were moved to tears as if an angel had quit the job of being a bright spot in their lives. After a few days, I wrote a tribute that appeared on my Website. For roughly a month I assembled photos and went thru Mom’s records finding amazing works she had created; from these I composed a viewfoil presentation and other memorial displays of ‘her time:’ the one-in-a-million life my mom had lived. In my own process of creation I came to see how absolutely notable she was, how alive she was to herself and to so many in so many eras and places. Talk about a hard act to follow!
Approximately a dozen of the people closest to her I invited to a ‘remembrance reception’ featuring the Mom discoveries it had been my pleasure to fashion into compositions. And as I stated in the eulogy and ceremony portion, “So many have been kind to say they are sorry for my loss. Yet, increasingly when I hear these words, I feel the more fitting sentiment is to salute me on my gain… for having been so fortunate to have had this woman in my life at all, and truly blessed to have had her as my mother.” Today I feel the sense of loss and the sense of gain are about even… with an edge to the latter as a surge of spiritual energy fills my being from the Source to which she’s returned.
In the book that proceeds from this series on ‘Omamacare,’ I shall add more observations on life and death in general, and Mom’s remarkable existence in particular. Also, because Omamacare has a focus on the modern health business, I’ll definitely discuss lessons learned: from the need for continuity and connection in any medical system worth its salt, to  what regular people can do to get the best treatment in such a system, to improving hospice care, and even to enhancing Henry Ford healthcare as a whole.
what regular people can do to get the best treatment in such a system, to improving hospice care, and even to enhancing Henry Ford healthcare as a whole.
It’s not all bad and we can do a whole lot better.
[1] The whole process of making preparations for what to do with the body upon death, and then what to expect in the conveyance of ‘cremains’ to its final resting place makes for interesting description. Also helpful, if you happen to find yourself in a low-budget freelance situation as I am; but I’ll save such details for the book.
[2] I’ve decided not to discuss in this column the probable nature of the various family disconnections from Mom; I may expand in the Omamacare book… when I can honestly state there is none of my ego in the exposure. I feel it is important for the reader to know that nothing Mom herself ever did rose to the level of a reason for any family member to disrespect or turn their backs on her.
[3] I should mention that Mom’s attitude toward being dissed by the offspring is what I call ‘constructively fatalistic.’ Though perplexed and hurt and finally resigned, she has always taken the high road. She chooses to focus on her valued silver-linings… on those few who do show up to hold her hand; on those who do send cards, letters, and much-appreciated comfort; on her little circle of well-wishers and caretakers and the myriad medical personnel whom she has known and loved over the years, and who, together with the others, have wholly loved her back.
This post has been read 3572 times!


What an ordeal you had. I am so lucky not to have gone through that in losing Nancy. May you have a brighter future.
You did right by her…….I think Forrest would would say so, too! Thanks for sharing!
Brian:
This was a beautiful story. I’m happy for your gain…in having such a woman in your life. Very moving.
D